COVID-19 severity affected by the proportion of antibodies targeting crucial viral protein
COVID-19 severity affected by the proportion of antibodies targeting crucial viral protein
COVID-19 antibodies preferentially target a different part of the virus in mild cases of COVID-19 than they do in severe cases and wane significantly within several months of infection, according to a new study by researchers at Stanford Medicine.
The findings identify new links between the course of the disease and a patient's immune response. They also raise concerns about whether people can be re-infected, whether antibody tests to detect prior infection may underestimate the pandemic's breadth, and whether vaccinations may need to be repeated at regular intervals to maintain a protective immune response.
"This is one of the most comprehensive studies to date of the antibody immune response to SARS-CoV-2 in people across the entire spectrum of disease severity, from asymptomatic to fatal," said Scott Boyd, MD, Ph.D., associate professor of pathology. "We assessed multiple time points and sample types, and also analyzed levels of viral RNA in patient nasopharyngeal swabs and blood samples. It's one of the first big-picture looks at this illness."
The study found that people with severe COVID-19 have low proportions of antibodies targeting the spike protein used by the virus to enter human cells compared with the number of antibodies targeting proteins of the virus's inner shell.
Boyd is a senior author of the study, which was published Dec. 7 in Science Immunology. Other senior authors are Benjamin Pinsky, MD, Ph.D., associate professor of pathology, Peter Kim, Ph.D., Virginia and D. K. Ludwig, and Biochemistry. The lead authors are research scientist Katharina Röltgen, Ph.D., postdoctoral scholars Abigail Powell, Ph.D., Oliver Wirz, Ph.D., and clinical instructor Bryan Stevens, MD.
The virus binds to the ACE2 receptor.
The researchers studied 254 people with asymptomatic, mild, or severe COVID-19 who were identified either through routine testing or occupational health screening at Stanford Health Care or who came to a Stanford Health Care clinic with symptoms of COVID-19. Of the people with symptoms, 25 were treated as outpatients, 42 were hospitalized outside the intensive care unit, and 37 were treated in the intensive care unit. Twenty-five people in the study died of the disease.
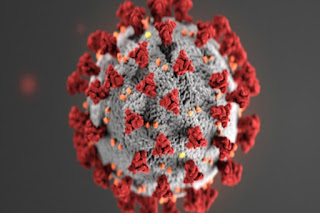
SARS-CoV-2 binds to human cells via a structure on its surface called the spike protein. This protein binds to a receptor on human cells called ACE2. The binding allows the virus to enter and infect the cell. Once inside, the virus sheds its outer coat to reveal an inner shell encasing its genetic material. The virus soon co-opts the cell's protein-making machinery to churn out more viral particles, which are then released to infect other cells.
Antibodies that recognize and bind to the spike protein block its ability to bind to ACE2, preventing the virus from infecting the cells. In contrast, antibodies that recognize other viral components are unlikely to prevent viral spread. Current vaccine candidates use portions of the spike protein to stimulate an immune response.
Boyd and his colleagues analyzed the levels of three types of antibodies -- IgG, IgM, and IgA -- and the proportions that targeted the viral spike protein or the virus's inner shell as the disease progressed and patients either recovered or grew sicker. They also measured the levels of viral genetic material in nasopharyngeal samples and blood from the patients. Finally, they assessed the antibodies' effectiveness in preventing the spike protein from binding to ACE2 in a laboratory dish.
"Although previous studies have assessed the overall antibody response to infection, we compared the viral proteins targeted by these antibodies," Boyd said. "We found that the severity of the illness correlates with the ratio of antibodies recognizing domains of the spike protein compared with other nonprotective viral targets. Those people with mild illness tended to have a higher proportion of anti-spike antibodies, and those who died from their disease had more antibodies that recognized other parts of the virus."
Substantial variability in the immune response
However, the researchers caution that although the study identified trends among a group of patients, there is still substantial variability in individual patients' immune response, particularly those with severe disease.
"Antibody responses are not likely to be the sole determinant of someone's outcome," Boyd said. "Among people with severe disease, some die, and some recover. Some of these patients mount a vigorous immune response, and others have a more moderate response. So, there are a lot of other things going on. There are also other branches of the immune system involved. It's important to note that our results identify correlations but don't prove causation."
As in other studies, the researchers found that people with asymptomatic and mild illness had lower levels of antibodies overall than did those with severe disease. After recovery, IgM and IgA levels decreased steadily to low or undetectable levels in most patients over a period of about one to four months after symptom onset or estimated infection date, and IgG levels dropped significantly.
"This is quite consistent with what has been seen with other coronaviruses that regularly circulate in our communities to cause the common cold," Boyd said. "It's not uncommon for someone to get re-infected within a year or sometimes sooner. It remains to be seen whether the immune response to SARS-CoV-2 vaccination is stronger or persists longer than that caused by natural infection. It's quite possible it could be better. But there are a lot of questions that still need to be answered."
Boyd is a co-chair of the National Cancer Institute's SeroNet Serological Sciences Network, one of the nation's largest coordinated research efforts to study the immune response to COVID-19. He is the principal investigator of the Center of Excellence in SeroNet at Stanford, which tackles critical questions about the mechanisms and duration of immunity to SARS-CoV-2.
"For example, if someone has already been infected, should they get the vaccine? If so, how should they be prioritized?" Boyd said. "How can we adapt seroprevalence studies in vaccinated populations? How will immunity from vaccination differ from that caused by a natural infection? And how long might a vaccine be protective? These are all fascinating, important questions."
Other Stanford co-authors of the study are visiting pathology instructor Catherine Hogan, MD; postdoctoral scholars Javaria Najeeb, PhD, and Ana Otrelo-Cardoso, PhD; medical resident Hannah Wang, MD; research scientist Malaya Sahoo, PhD; research professional ChunHong Huang, PhD; research scientist Fumiko Yamamoto; laboratory director Monali Manohar, PhD; senior clinical laboratory scientist Justin Manalac; Tho Pham, MD, clinical assistant professor of pathology; medical fellow Arjun Rustagi, MD, PhD; Angela Rogers, MD, assistant professor of medicine; Nigam Shah, PhD, professor of medicine; Catherine Blish, MD, PhD, associate professor of medicine; Jennifer Cochran, PhD, chair and professor of bioengineering; Theodore Jardetzky, PhD, professor of structural biology; James Zehnder, MD, professor of pathology and of medicine; Taia Wang, MD, PhD, assistant professor of medicine and of microbiology and immunology; senior research scientist Balasubramanian Narasimhan, PhD; pathology instructor Saurabh Gombar, MD, PhD; Robert Tibshirani, PhD, professor of biomedical data science and of statistics; and Kari Nadeau, MD, PhD, professor of medicine and of pediatrics.
The study was supported by the National Institutes of Health (grants RO1AI127877, RO1AI130398, 1U54CA260517, T32AI007502-23, U19AI111825, and UL1TR003142), the Crown Family Foundation, the Stanford Maternal and Child Health Research Institute, the Swiss National Science Foundation, and a Coulter COVID-19 Rapid Response award.
Boyd, Röltgen, Kim, and Powell have filed provisional patent applications related to serological tests for SARS-CoV-2 antibodies.



Comments
Post a Comment